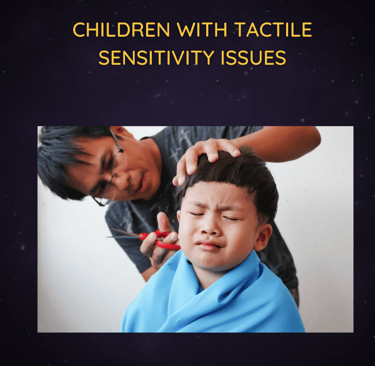
When Touch Feels Too Much: Understanding Tactile Sensitivity in Neurodivergent Children
For some children, touch isn’t comforting—it’s overwhelming. Tactile sensitivity in neurodivergent kids can lead to meltdowns, avoidance, and academic struggles. Learn how it shows up, why it matters, and how early occupational therapy can help children feel safe and confident in their world.

When Touch Feels Too Much: Understanding Tactile Sensitivity in Neurodivergent Children
Introduction
Imagine cringing at the feel of your clothes, recoiling at a classmate’s accidental touch, or panicking at the thought of finger-painting. For many neurodivergent children, this is their daily experience. What looks like defiance, fussiness, or odd behavior is often the result of tactile sensitivity—a sensory processing challenge that can severely impact comfort, learning, and social interaction.
Tactile sensitivity is especially common in children with Autism, Sensory Processing Disorder (SPD), ADHD, and Anxiety-related conditions. And while it’s often misunderstood, the good news is that early occupational therapy intervention can empower children to feel safe in their bodies and environments.
👋 What Is Tactile Sensitivity?
Tactile sensitivity—also called tactile defensiveness—occurs when the nervous system overreacts to touch sensations that are typically harmless or neutral. These sensations may include:
Clothing textures
Tags and seams
Hair brushing or washing
Certain foods
Hands-on activities like clay, glue, or sand
Physical proximity with peers
Children may respond with discomfort, avoidance, or even distress to these inputs. Their brain interprets them as threats, triggering a “fight or flight” reaction.
🚸 How It Presents in School-Going Children
Tactile sensitivity can affect every aspect of a school day—from getting dressed in the morning to joining in classroom activities.
Common signs include:
Refusal to wear certain clothing (e.g., socks, collars, jeans)
Meltdowns or anxiety around hair brushing, handwashing, or face wiping
Avoidance of messy play, crafts, or touching new textures
Pulling away from physical contact—e.g., high-fives or hugs
Difficulty standing in lines or sitting on carpet squares
Extreme reactions to accidental bumps or touch from peers
Constant adjusting or tugging at clothing
Fear of certain activities like sand, finger paint, or glue
These children are not being difficult—they are in genuine sensory distress.
🧠 Who Is Affected?
Tactile sensitivity is especially common in children with:
Autism Spectrum Disorder (ASD): Sensory differences are a core feature of autism, and tactile defensiveness is often one of the most noticeable traits.
Sensory Processing Disorder (SPD): Children may be hypersensitive to touch while being under-responsive in other areas.
ADHD: Sensory issues can coexist, and tactile defensiveness can add to restlessness and distractibility.
Anxiety Disorders: Heightened stress can make tactile stimuli feel more threatening than they are.
Tactile sensitivity is not a behavioral choice—it is a sensory regulation issue.
📉 The Impact of Tactile Sensitivity on Learning and Wellbeing
Tactile defensiveness can interfere with a child’s ability to participate in everyday activities that are foundational to learning and social development.
1. Academic Challenges:
Refusal to engage in hands-on tasks like art, science experiments, or handwriting
Avoidance of group activities that involve close contact
Disruption in learning routines due to sensory overload
2. Emotional Impact:
Chronic anxiety or irritability
Meltdowns during transitions or dressing tasks
Low self-esteem and fear of failure
3. Social Withdrawal:
Avoidance of peers or group play
Fear of touch leads to isolation
Misinterpretation by teachers or peers as being "aloof" or “aggressive”
4. Physical Limitations:
Resistance to haircuts, toothbrushing, or bathing
Limited exposure to sensory-rich activities that build fine motor skills
Without support, children may begin to internalize shame or anxiety, leading to long-term emotional and developmental consequences.
💡 Why Early Occupational Therapy Matters
The earlier tactile defensiveness is identified, the better. Occupational therapists are trained to help children understand their sensory needs and gradually build tolerance through structured, supportive activities.
Early OT support helps children feel safe in their bodies, more comfortable in group settings, and better able to participate in everyday school and home life.
🛠️ How Occupational Therapy Helps
Occupational therapy for tactile sensitivity typically focuses on sensory integration—a structured process of exposing the child to various textures and touch inputs in a way that feels safe and manageable.
OT approaches include:
1. Desensitisation Techniques:
Introducing textures slowly through play (e.g., shaving cream art, water beads, dry rice bins)
Using firm touch or deep pressure to override light, alerting sensations
Gradual exposure to previously avoided clothing or grooming routines
2. Sensory Diets:
Daily routines of touch-based activities to regulate the nervous system (e.g., brushing protocols, deep pressure games, skin-safe massage)
3. Environmental Modifications:
Removing tags from clothes, softening seams, allowing for preferred textures
Creating sensory-friendly classrooms (e.g., seating options, calm corners)
4. Emotional Support and Coping Skills:
Teaching children to name their discomfort and ask for help
Using visuals and social stories to prepare them for sensory tasks
Reframing anxiety around tactile input as something they can manage—not fear
5. Parent and Teacher Guidance:
Helping adults understand that the child’s reactions are not defiance
Creating consistent strategies across home and school
🧒 Real Story: Maya’s Touch Troubles
Maya, age 7, hated socks and couldn’t tolerate writing with a pencil. She refused finger painting and cried every morning about her school uniform. Her teacher labelled her “defiant,” and her parents felt helpless.
After a sensory-based OT assessment, Maya was diagnosed with tactile defensiveness. With a tailored sensory diet, play-based exposure to textures, and adaptations to her clothing, Maya began engaging in class activities—and even smiled during art class.
👨🏫 What Parents and Teachers Can Do
Tactile sensitivity is not something children "grow out of"—but they can grow with support.
Steps to take:
Observe: Identify what textures or touch experiences seem to trigger distress
Document Patterns: When and where does it happen? What helps or worsens it?
Speak Up: Share concerns with teachers and request an OT referral if needed
Adapt: Allow sensory-friendly clothing options, avoid forced hugs or hand-holding, and respect touch boundaries
Support Gradually: Encourage play that explores texture in a safe way (e.g., water play, kinetic sand, soft cloths)
Educate Yourself: Use resources like Newbee Publication's sensory support guides or apps like Locus Therapy to screen and support sensory needs
🧾 Conclusion
Tactile sensitivity may seem like a minor issue—but for a child, it can mean the difference between participation and panic. Understanding this form of sensory processing difference is the first step toward creating calm, inclusive, and empowering environments.
With early occupational therapy and supportive adults, children can learn to manage their tactile challenges—and thrive in their own skin.